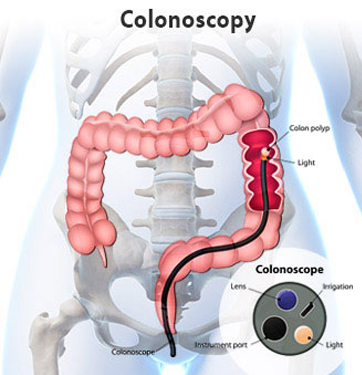
For the procedure, you will lie on your left side on the examining table. You will be given pain medication and a mild sedative to keep you comfortable and to help you relax during the exam. The physician will insert a long, flexible, lighted tube into your rectum and slowly guide it into your colon. The tube is called a colonoscope. The scope transmits an image of the inside of the colon onto a monitor, so the physician can carefully examine the lining of the colon. The scope bends, so the physician can move it around the curves of your colon. You may be asked to change position occasionally to help the physician move the scope. The scope also blows air into your colon, which inflates the colon and helps the physician see better.
If anything unusual is in your colon, like a polyp or inflamed tissue, the physician can remove it or a piece of it using tiny instruments passed through the scope. That tissue (biopsy) is then sent to a lab for testing. If there is bleeding in the colon, the physician can use the scope to pass a laser, heater probe or electrical probe, or inject special medicines, to stop the bleeding.
Colonoscopy takes 30 to 60 minutes. The sedative and pain medicine should keep you from feeling much discomfort during the exam. You will need to remain at the facilty for 1 to 2 hours until the sedative wears off and you will need someone to drive you home.